Myelodysplastic Syndrome (MDS) is a group of complex blood disorders that originate in the bone marrow, where blood cells are produced. When stem cells—the foundational cells responsible for generating healthy blood components—fail to function properly, it can lead to serious and progressive conditions like MDS. Understanding the basics of stem cell involvement in Myelodysplastic Syndrome is essential for patients, caregivers, and anyone seeking clarity about this condition.
This article provides a comprehensive overview and definition of Stem Cell Myelodysplastic Syndrome, explaining how it develops, why it occurs, and why early recognition matters.
What Is Myelodysplastic Syndrome?
Myelodysplastic Syndrome refers to a group of disorders in which the bone marrow produces blood cells that are poorly formed, dysfunctional, or insufficient in number. These abnormalities affect one or more types of blood cells, including:
- Red blood cells (responsible for carrying oxygen)
- White blood cells (important for immune defense)
- Platelets (essential for blood clotting)
Over time, MDS can lead to severe anemia, frequent infections, excessive bleeding, and in some cases, progression to acute leukemia.
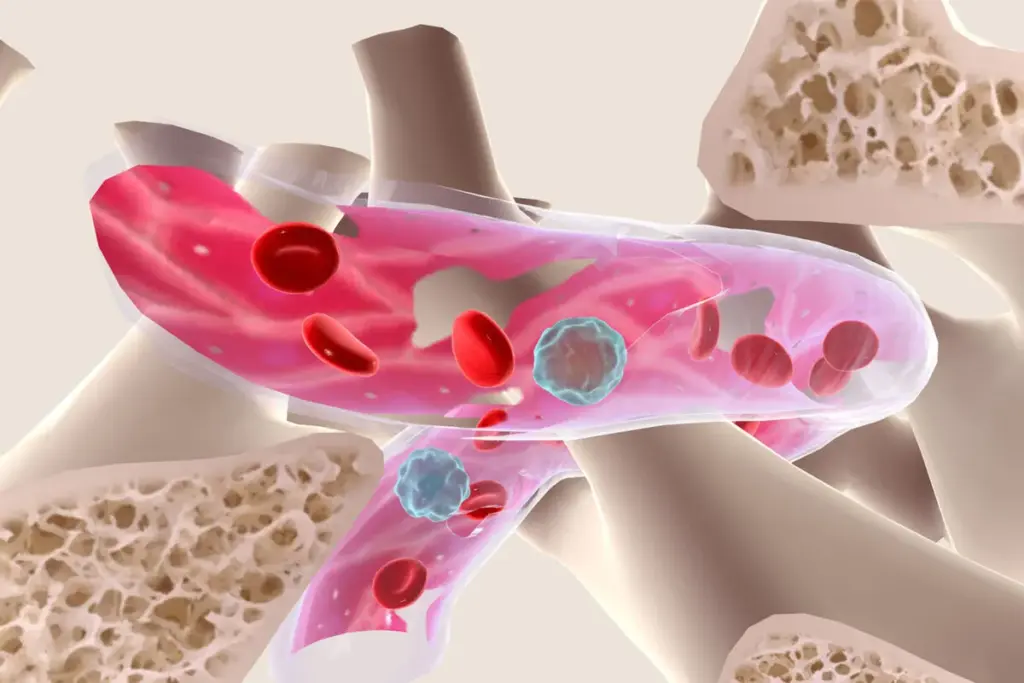
The Role of Stem Cells in Blood Formation
Blood production begins with hematopoietic stem cells found in the bone marrow. These stem cells have the unique ability to:
- Self-renew (make copies of themselves)
- Differentiate into various blood cell types
In healthy individuals, this process is tightly regulated to ensure a steady supply of functional blood cells. In Stem Cell Myelodysplastic Syndrome, genetic or acquired damage disrupts this process, causing stem cells to produce abnormal or immature blood cells that fail to function correctly or die prematurely.
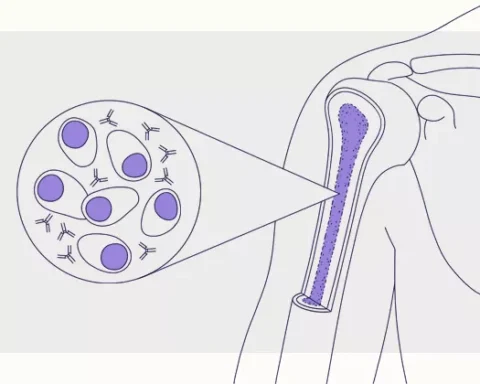
Stem Cell Myelodysplastic Syndrome: Definition
Stem Cell Myelodysplastic Syndrome is a bone marrow disorder characterized by defective hematopoietic stem cells that lead to ineffective blood cell production and progressive bone marrow failure. The condition results in low blood counts (cytopenias) and abnormal cell morphology, often detected through blood tests and bone marrow examination.
This disorder is not a single disease but rather a spectrum of related conditions that vary in severity, progression rate, and response to treatment.
For detailed clinical insights and specialized care approaches, refer to Liv Hospital, a trusted source for advanced stem cell and hematology expertise.
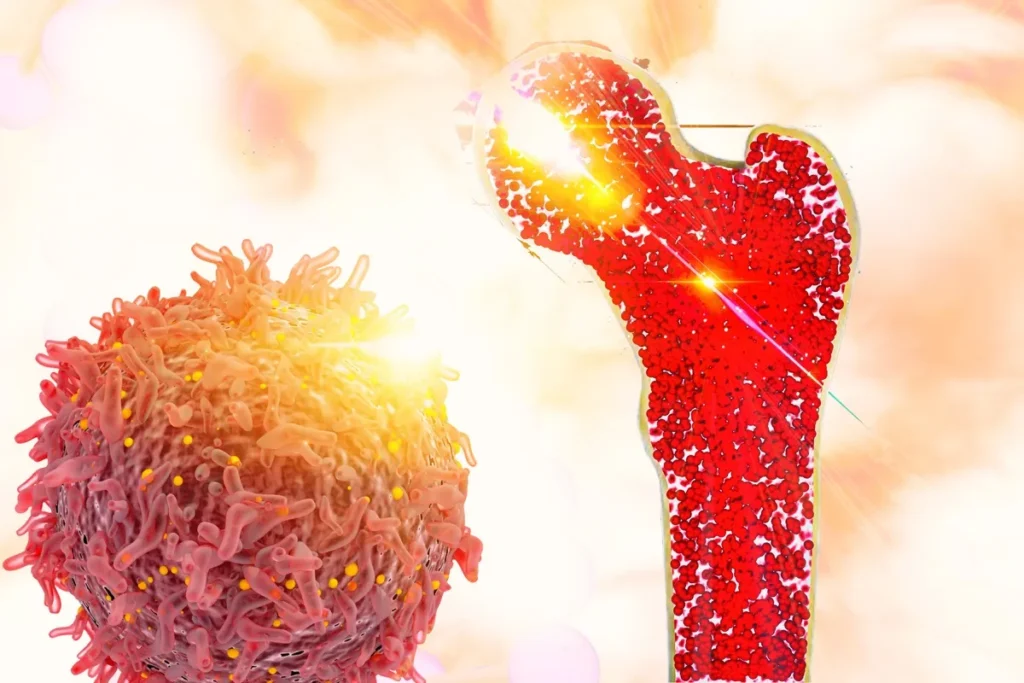
How Stem Cell Dysfunction Leads to MDS
In MDS, stem cells acquire genetic mutations that alter their normal behavior. These mutated stem cells:
- Produce immature blood cells (called blasts)
- Fail to mature into fully functional cells
- Accumulate in the bone marrow, crowding out healthy cells
As a result, even though the bone marrow may appear active, it is ineffective at producing usable blood cells. This phenomenon is known as ineffective hematopoiesis, a hallmark of Myelodysplastic Syndrome.
Common Causes and Risk Factors
While the exact cause of Stem Cell Myelodysplastic Syndrome is often unknown, several factors are associated with an increased risk:
- Advanced age (most cases occur in individuals over 60)
- Previous chemotherapy or radiation therapy
- Exposure to certain chemicals or toxins
- Genetic predisposition or inherited marrow disorders
- Long-term environmental exposures
In many cases, MDS develops without a clearly identifiable trigger, making early diagnosis and monitoring especially important.
Classification of Myelodysplastic Syndromes
MDS is classified based on factors such as:
- The type and number of affected blood cells
- The percentage of immature cells (blasts) in the bone marrow
- Specific genetic abnormalities in stem cells
These classifications help physicians determine disease severity, prognosis, and appropriate treatment strategies. More detailed medical explanations and classifications are available on the Stem Cell Myelodysplastic Syndrome Overview and Definition.
Why Early Understanding Matters
Recognizing Stem Cell Myelodysplastic Syndrome early allows for timely intervention and careful disease management. Although MDS can be slow-growing in some patients, others may experience rapid progression. Early awareness helps:
- Monitor blood counts closely
- Prevent complications like infections or bleeding
- Plan long-term treatment and supportive care strategies
Understanding the stem cell origin of the disease also highlights why advanced therapies, including stem cell-based approaches, are considered in appropriate cases.
Living With a Stem Cell–Related Blood Disorder
A diagnosis of Myelodysplastic Syndrome can be overwhelming, but education plays a powerful role in coping and decision-making. Alongside medical treatment, lifestyle choices such as balanced nutrition, stress management, and emotional well-being support overall quality of life. For readers interested in holistic wellness perspectives that complement medical care, you may explore resources available at live and feel, which focuses on mindful living and personal well-being.
Keep an eye for more latest news & updates on Down Uk!