Multiple myeloma is a complex blood cancer that affects plasma cells in the bone marrow. Over the past few decades, treatment outcomes for multiple myeloma have improved significantly, largely due to advances in stem cell–based therapies. Stem cell treatment plays a crucial role in controlling the disease, prolonging remission, and improving quality of life for eligible patients.
At advanced healthcare centers such as Liv Hospital, stem cell therapies for multiple myeloma are delivered using evidence-based protocols, advanced technology, and multidisciplinary expertise.
Understanding Multiple Myeloma and the Role of Stem Cell Therapy
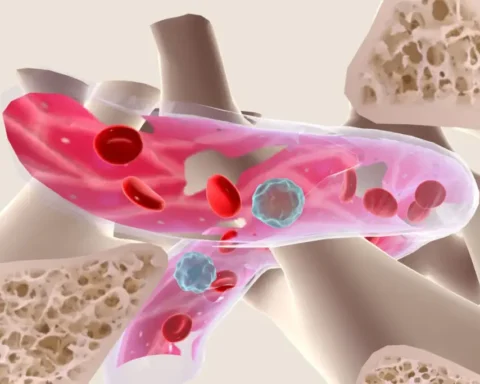
Multiple myeloma occurs when abnormal plasma cells multiply uncontrollably, crowding out healthy blood-forming cells. This can lead to bone damage, anemia, kidney problems, and weakened immunity.
Stem cell therapy is not a cure, but it is considered one of the most effective treatments for achieving long-term remission. It works by allowing doctors to use high-dose chemotherapy to destroy cancer cells, followed by stem cell infusion to restore healthy bone marrow function.
Who Is Eligible for Stem Cell Treatment?
Stem cell treatment is typically recommended for patients who:
- Are newly diagnosed and medically fit
- Have responded well to initial (induction) therapy
- Have adequate heart, lung, liver, and kidney function
- Are generally under a certain age threshold, although biological fitness matters more than chronological age
Each patient undergoes a detailed evaluation before being considered for stem cell procedures.
Types of Stem Cell Transplants Used in Multiple Myeloma
Autologous Stem Cell Transplant (ASCT)
This is the most common stem cell procedure for multiple myeloma. It uses the patient’s own stem cells.
Why it’s preferred:
- Lower risk of immune complications
- Faster recovery compared to donor-based transplants
- Proven effectiveness in extending remission
Allogeneic Stem Cell Transplant
This involves stem cells from a compatible donor. While less commonly used due to higher risks, it may be considered in select cases, particularly for younger patients or those with aggressive disease.
Step-by-Step Stem Cell Multiple Myeloma Treatment Procedures
For a comprehensive clinical overview, patients and caregivers can explore Stem Cell Multiple Myeloma Treatment and Procedures in detail. Below is a simplified explanation of the process.
1. Induction Therapy
Treatment begins with combination drug therapy to reduce the number of myeloma cells. This phase helps prepare the body for stem cell collection and transplant.
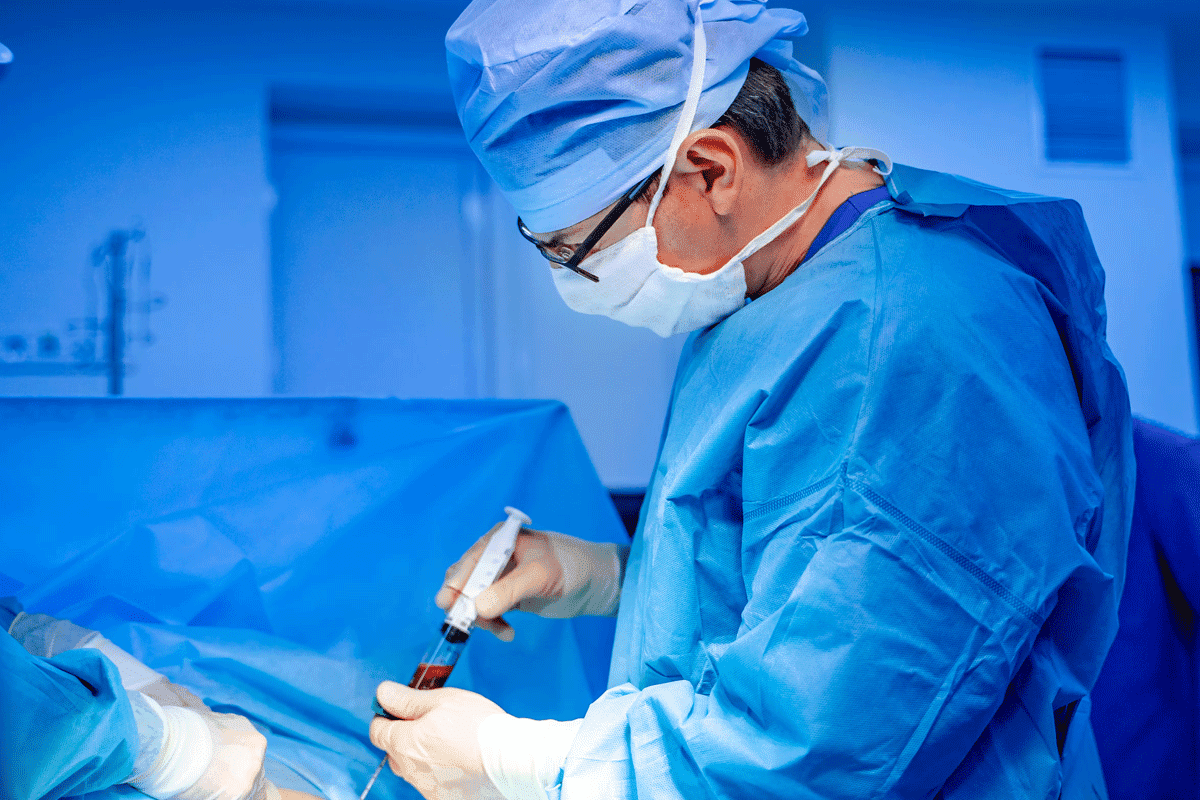
2. Stem Cell Mobilization and Collection
Medications are given to stimulate stem cells to move from the bone marrow into the bloodstream. These stem cells are then collected using a specialized procedure called apheresis and safely stored.
3. High-Dose Chemotherapy
Once stem cells are collected, patients receive high-dose chemotherapy designed to eliminate remaining cancer cells. This treatment also destroys existing bone marrow, making stem cell infusion essential.
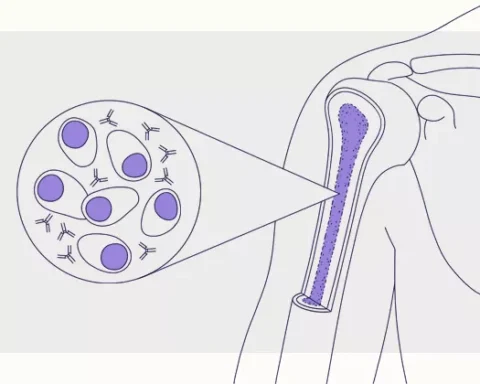
4. Stem Cell Infusion
The stored stem cells are infused back into the patient through a vein, similar to a blood transfusion. These cells travel to the bone marrow and begin regenerating healthy blood cells.
5. Engraftment and Recovery
Engraftment occurs when the transplanted stem cells start producing new blood cells. This phase typically takes 2–3 weeks and requires close medical monitoring to manage infection risk and side effects.
Post-Transplant Care and Monitoring
Recovery does not end with discharge from the hospital. Ongoing follow-up includes:
- Regular blood tests
- Infection prevention strategies
- Maintenance therapy to prolong remission
- Bone health monitoring
- Lifestyle guidance to support immune recovery
Long-term follow-up is essential for detecting relapse early and managing late effects of treatment.
Benefits of Stem Cell Therapy in Multiple Myeloma
Stem cell treatment offers several advantages:
- Deeper and longer-lasting remission
- Improved overall survival rates
- Better disease control when combined with modern drug therapies
- Enhanced quality of life for many patients
Outcomes depend on individual health, disease stage, and response to prior treatments.
Potential Risks and Side Effects
While effective, stem cell procedures may involve risks such as:
- Temporary immune suppression
- Infection
- Fatigue and nausea
- Organ-related side effects
- Rare transplant-related complications
These risks are carefully managed through specialized supportive care and continuous monitoring.
Living Well After Treatment
Life after stem cell treatment for multiple myeloma focuses on recovery, emotional well-being, nutrition, and physical strength. Patients are encouraged to adopt healthy habits, manage stress, and stay informed about long-term care. Supportive resources that focus on balanced living, mindfulness, and wellness—such as live and feel can be helpful during the survivorship journey as patients work toward restoring normalcy and overall well-being.
Keep an eye for more latest news & updates on Down Uk!